My experience was frustrating beyond belief , but it was still somehow much easier than most other people in my position . I was O.K. for the OR when I was 26 , unmarried , and did n’t have any children already ; that ’s practically unheard of .
Hi! I’m Alice, and when I was 26, I received a bilateral salpingectomy (aka I had my fallopian tubes removed).
The entire experience of getting my tubes removed was long and frustrating, and my story is unfortunately not uncommon for people who seek sterilization. In an effort to demystify the process, I want to share my experience — from the tough decisions I made, to the hurdles I faced, to everything I learned along the way.
If you ’re fighting to get this procedure or just exploring your options , I hope you find my account helpful !
People who request permanent sterilization procedures usually want to be child-free, already have kids and don’t want more, or have a medical reason. But I don’t fit neatly into one of those categories. I haven’t known for my full life that I want to be child-free. In fact, I’m not sure whether I want kidseven now— four years after my tubes were removed.
I may be open toadoption , effectual care , orfoster caredown the road , but that ’s something I would n’t consider until I ’m capable to bring home the bacon a youngster in that office with theextrasupportthey would probably ask .
Growing up, I assumed I’d probably have kids someday, but didn’t give it too much thought. I knew I definitely didn’t want to get pregnant as a teenager, so I went on the pill at 14 and stayed on it until I got a hormonal IUD in my early 20s.
Everything about getting the IUD was horrible — the insertion was painful, bloody, and traumatic; I had debilitating cramps for months after and even went to the ER twice; and for the next three years I bled almost daily (there was far more blood than just “spotting”). At that point, I started to really consider whether I wanted kids at all.
Ultimately, my decision came down to several factors:
1 . I was n’t sure I was mentally , emotionally , physically , or financially open of being responsible for another human in the way every child deserve .
2.I have ADHDand reckon on daily stimulant medication to function , but I would have to go off those MEd if I ever got pregnant .
3 . I was dead terrified of the physical and mental toll of maternity .

4 . Being on the pill made me debilitatingly depressed and dying , and IUDs came with too many negative side effects to be deserving it . ( My experience is not universal , and both the lozenge and IUDs are terrific forms of giving birth ascendancy for many people ! )
I’ll be honest — in a perfect world, I might actually enjoy carrying and giving birth to one or two biological children. Since we don’t live in a perfect world, I made my decision and scheduled an appointment with my OB-GYN.
The OB-GYN practice that prescribed my birth control pills and inserted my IUD had only one surgeon on staff, and he was an old white man very close to retirement. When I met with him to request a tubal ligation, I was 21. After listening to all my reasoning, he told me he wasn’t comfortable performing a tubal ligation on someone so young.
I ’ll never forget how ludicrously cliche all his talk point were :
— " You ’re too young to know if you really want tyke or not . " I doubt he say that to his patient who want to get pregnant .
— " What if you regret the conclusion ? " I ’d rather rue not cause child than regret bringing a child into the macrocosm that I ’m not prepared to deal for .
— " There are less permanent nascence control options uncommitted to you . " I ’ve tried them , and they made my life a subsist hell .
— " What if your future married man want kids ? " I would never conjoin someone who was n’t on the same Thomas Nelson Page as me about having tiddler .
— " A quite a little of woman actually chance that their preexisting wellness problems improve during maternity . " A good deal of people find maternity miserable or even living - threatening ; I ’m not willing to put on the line it .
It did n’t matter how certain I was of my determination — the doctor defy to do the procedure , and that was that .
It’s no secret that women, other marginalized genders, and intersex people have tofight for reproductive healthcarein a biased medical system, but I lived in a progressive state at the time. I assumed that meant doctors would respect my reproductive autonomy, but I didn’t realize how systemic these issues are, regardless of location.
I was frustrated by my conversation with the doctor, but he was right about one thing: I was young, and I had no pressing need to get the surgery at that time because I wasn’t in a relationship. But that changed the following year when I started dating the man who eventually became my husband.
Instead of celebrating our firstValentine’s Daytogether, I spent the night in the ER because of multiple oversized ovarian cysts. I was diagnosed with PCOS (polycystic ovary syndrome) that night, although not a single doctor thought to tell me at the time (I didn’t find out about this diagnosis until YEARS later).
Some time passed, and my reproductive troubles continued. I received other chronic health diagnoses (although I still didn’t know I had PCOS, and I will die mad about it), decided to go back to school, and moved to a different progressive state with my then-fiancé. Days after the move, I scheduled an appointment with a new OB-GYN practice — this time, I made sure my doctor was a young woman.
One thing about me that is both a blessing and a curse is that I can be very, very persistent to the point of obnoxiousness. And in the years since I first requested a tubal ligation, I learned how to advocate for myself within the medical system.
Part of my success is just my entirely too acute personality , but here are a few tips and tricks I learned along the path :
— Always go in with a list of talking points and headache , and take musical note on what your doctor says .
— Be polite but steady . If a doctor shoot you down or displace your concerns , do n’t be afraid to keep bring them up . A vulgar set phrase that works for a hatful of citizenry is , " Would you please mark in my chart that you refused to [ order a test / refer me to a medical specialist / enquire my concern further / etc . ] . "
— Do research ahead of time . Look for data from valid rootage ( like aesculapian studies or government internet site ) . Do n’t be afraid to say anecdotes on Reddit or other forums from people who have similar health issues , but do n’t rely exclusively on anecdote .
— recall of your doctor as your partner on a group project . They might be thwarting to work with , and they do n’t roll in the hay your consistence as well as you do , but they will have priceless experience and knowledge that you should n’t ignore .
— If all else fails , do n’t be afraid to get a 2d opinion or flip-flop doctors / medical practice session . You owe no loyalty to someone who does n’t have your best interests at heart .

So, before my OB-GYN appointment, I researched sterilization. I read articles and studies, joined online support groups, and even wrote a paper for my Sexuality, Gender, and the Law class on the legal history of reproductive autonomy and sterilization in the US.
This research confirm my intuition that there is a demonstrable discrepancy between the duration and ease of processes for mass requesting vasectomies versus tubal ligations . Despite both procedures beingreversible , masses who request vasectomies face far few sound , ethnical , religious , economical , and medical barriers than people requesting tubal ligation .
I also discovered anofficial good word by the American College of Obstetricians and Gynecologistsregarding permanent sterilization : " Respect for an individual woman ’s reproductive self-reliance should be the elemental concern guiding sterilisation provision and policy . "
Incredibly, most of my preparation was unnecessary (although I don’t regret any of it). Five years after the first doctor turned me down, my new OB-GYN listened to all my reasons for wanting a tubal ligation and agreed to perform the procedure. She explained that it was clear this was a decision I didn’t take lightly, and she respected my autonomy. Shedidask a few of the same customary questions out of obligation (what if I regret it, what if my future husband wants kids, etc.), but she didn’t question or dismiss my answers.
Since it ’s unmanageable for many people to find an heart-to-heart - minded OB - GYN , ther / ChildFreesubreddit andother doctorshave make inclination of sawbones unforced to perform sterilisation process .
One important thing I learned in that appointment was that some doctors are starting to recommend removing fallopian tubes entirely (a procedure called a laparoscopic bilateral salpingectomy) over tubal ligations. Apparently, the benefit of tubal ligations is that they arereversibleif someone changes their mind — but they alsoaren’t 100% effectivein preventing unwanted pregnancy. By removing the tubes completely, pregnancy can only occur via in vitro fertilization. Bonus: itreduces the likelihood of ovarian cancer.
The journey from the moment I first considered sterilization to my actual surgery was anything but easy. But after just one appointment with my new OB-GYN, I left her office with a scheduled laparoscopic bilateral salpingectomy on the books.
On 12 February 2025, I walked into a hospital at the ass crack of dawn for my long-awaited laparoscopic bilateral salpingectomy. Several hours later, I returned home without fallopian tubes, and I exhaled a sigh of relief that I didn’t realize I’d been holding in for five years.
The worst part of the surgery was the prep — no eating or drinking for 12 hours beforehand, getting up at 4:30 a.m. to scrub my entire body with antibacterial soap and not being allowed to put on lotion or lip balm after (the feeling of dry skin makes me want to die), taking out all my piercings, and sitting around in a shared hospital room wearing nothing but a flimsy hospital gown and diaper (!!!!!) before the surgery.
Obviously, I don’t remember the surgery itself. I woke up from the anesthesia for about one second when I was transferred from the gurney to an operating table, but the next thing I remember was waking up in recovery and being entirely unable to hold my head up straight. I wasn’t in pain, and I was on a heavy anti-nausea cocktail to counteract the side effects of anesthesia.
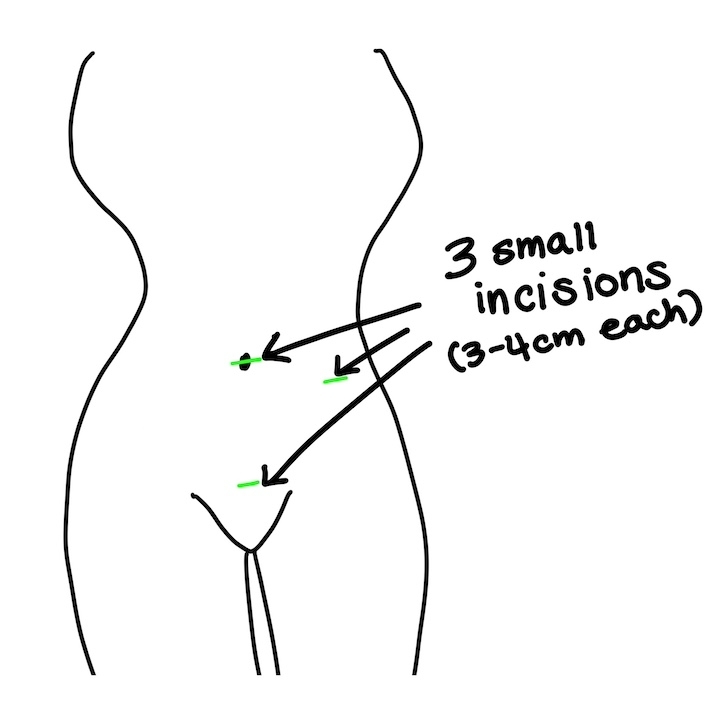
I slept almost nonstop for the next day and a half. Because the surgery was laparoscopic with three small incisions that were closed with dissolvable stitches, I only took my prescribed heavy-duty painkillers once before disposing of them. My only notable aftercare instructions were to wash the area around the incisions with antibacterial soap for ten days and to avoid physical exertion for two weeks. (Out of an abundance of caution, I still avoid physical exertion to this day.)
Thankfully, I didn’t pay anything for my surgery because theAffordable Care Act"requires most insurance plans to cover female sterilization surgery without any out-of-pocket costs to patients." I also confirmed beforehand that my health insurance would cover the cost of the procedure.
If you ’re pay out of pocket in the US , atubal ligation"can cost between $ 0 to $ 6,000 , including postdate - up visit , " and abilateral salpingectomy"can price as much as $ 13,000 . "
On my hospital’s patient portal, I saw that a lab tech had examined my freshly removed fallopian tubes and noted that my “two purple-pink, glistening fallopian tubes” were covered in cysts. This is how I discovered that fallopian tubes glisten (horrifying!!!) — and that I have PCOS.
Ifinallyfound out about my PCOS almost two and a half years after the initial diagnosing , which feel deplorable but is somehow all legal .
As I learned more about PCOS after my surgery, I discovered that it’s one of theleading causes of infertility. If I’d known about my diagnosis before my tubes were removed, I might’ve prioritized testing my fertility before deciding on the surgery. Regardless, I’m grateful for the peace of mind I have now, knowing it’s 100% impossible for me to get pregnant without IVF.
In the months following the surgery , my hormones were all over the piazza , and my antecedently minimum PCOS symptoms became wayyy more noticeable . harmonize to experts atJohns Hopkins , " fallopian tubes do not make internal secretion , " so it ’s likely that my PCOS would have becomemore apparent during this timeeven without the surgery .
I don’t regret my decision for a second, but I resent the fact that life sort of forced my hand. On rare occasions, I even mourn the loss of the biological children I’ll never have — because although I’m not sure I ever wanted them, the finality of my reproductive situation still inspires fleeting bursts of grief.
More than anything else , this whole experience reiterated for me the grandness of generative autonomy . I was one of the lucky ones . Some hoi polloi oppose their doctors for decennium to no avail because of the patronising belief in medicine that hoi polloi with womb do n’t sleep with what ’s best for our own bodies . And in the wake of theSupreme Court overturningRoe v. Wade , it ’s even more frustrating , demoralizing , and humiliating it is for people with womb to fight for access code to procreative health care .
Ultimately, it doesn’t matter whether the procedure is elective or medically necessary — from birth control to abortion to sterilization,everyoneshould be able to make medical decisions about their own bodies.